The system mimics real-world clinical workflows to enhance early diagnosis and monitoring of skin diseases, including melanoma.
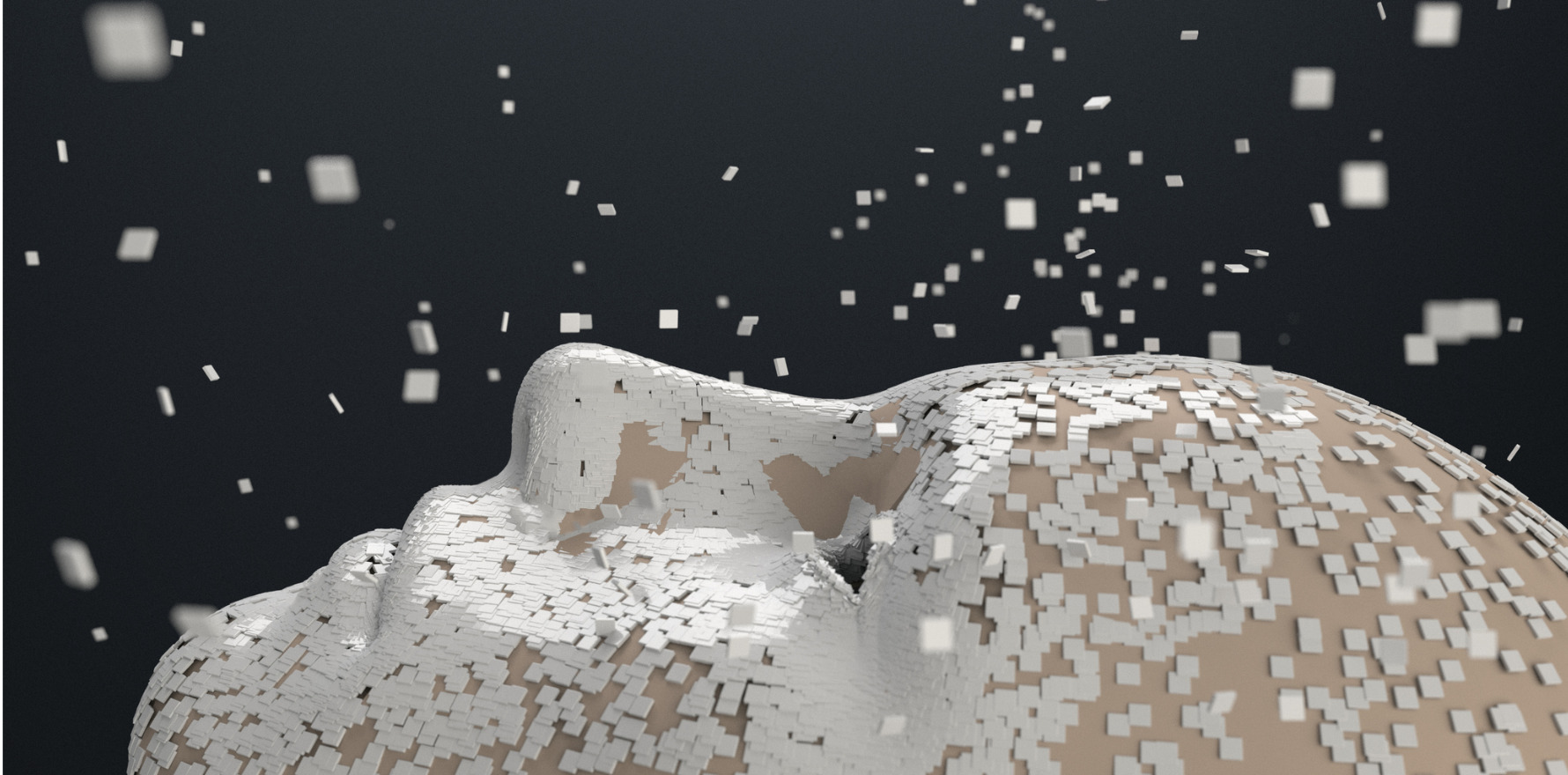
A new artificial intelligence tool developed by an international research consortium led by Monash University is set to transform dermatological diagnostics by enhancing speed and accuracy in identifying melanoma and a wide range of other skin diseases.
PanDerm is one of the first AI models designed to replicate and support real-world dermatological decision-making.
Unlike previous AI tools focused on narrow tasks such as analysing only dermoscopic images, PanDerm simultaneously evaluates multiple imaging modalities, including close-up photos, dermoscopy, pathology slides and total body photography.
An article published this month in Nature Medicine, details the new system and how it was developed and evaluated.
The research was led by AI and machine learning experts at the Monash AIM for Health Lab at Monash’s Faculty of Information Technology in collaboration with researchers and clinicians at Alfred Health, The University of Queensland, Medical University of Vienna, NVIDIA AI Technology Centre in Singapore, Princess Alexandra Hospital in Brisbane, University of Florence, Royal Prince Alfred Hospital, NSW Health Pathology and Hospital General Universitario de Alicante in Spain.
PanDerm was trained using over two million images sourced from 11 institutions across multiple countries, encompassing four major types of skin imaging. This multimodal approach allows the model to mimic how clinicians synthesize different visual cues in practice.
A series of evaluations showed PanDerm improved skin cancer diagnosis accuracy by 11% when used by doctors. The model helped non-dermatologist healthcare professionals improve diagnostic accuracy on various other skin conditions by 16.5%.
It also showed the ability to detect skin cancer early, identifying concerning lesions before clinician detection, an advancement that could significantly enhance early intervention.
In addition to skin cancer diagnosis and screening, the authors found PanDerm supported a wide range of dermatological tasks, including:
- Lesion monitoring and mole counting
- Risk prediction of cancer recurrence or metastasis
- Diagnosis of inflammatory and infectious skin conditions
- Lesion segmentation and skin type analysis
AI and computer vision expert and one of the lead co-authors of the research, Associate Professor Zongyuan Ge from Monash University’s Faculty of Information Technology, said existing AI models for dermatology remain limited to isolated tasks, such as diagnosing skin cancer from dermoscopic images; magnified images of skin captured using a dermoscope.
“Previous AI models have struggled to integrate and process various data types and imaging methods, reducing their usefulness to doctors in different real-world settings,” Associate Professor Ge said.
“PanDerm is a tool designed to work alongside clinicians, helping them interpret complex imaging data and make informed decisions with more confidence.”
First author and PhD student Siyuan Yan from Monash University Faculty of Engineering said the multimodal approach was key to the system’s success.
“By training PanDerm on diverse data from different imaging techniques, we’ve created a system that can understand skin conditions the way dermatologists do; by synthesising information from various visual sources,” Mr Yan said.
“This allows for more holistic analysis of skin diseases than previous single-modality AI systems.”
University of Queensland Dermatology Research Centre Director and one of the lead co-authors of the research, Professor Peter Soyer, said differences in imaging and diagnosis techniques could also arise due to different levels of resources available in urban, regional and rural healthcare spaces.
“The strength of PanDerm lies in its ability to support existing clinical workflows,” Professor Soyer said.
“It could be particularly valuable in busy or resource-limited settings, or in primary care where access to dermatologists may be limited.
“We have seen that the tool was also able to perform strongly even when trained on only a small amount of labelled data, a key advantage in diverse medical settings where standard annotated data is often limited.”
Lead co-author, Alfred Health Victorian Melanoma Service director, Professor Victoria Mar, said PanDerm showed promise in helping detect subtle changes in lesions over time and provide clues to lesion biology and future risk of spread.
“This kind of assistance could support earlier diagnosis and more consistent monitoring for patients at risk of melanoma,” Professor Mar said.
“In hospitals or clinic settings, doctors use diverse ways and different types of images to diagnose skin cancer or other skin conditions.”
Senior co-author Professor Harald Kittler from Medical University of Vienna Department of Dermatology said PanDerm demonstrated how global collaboration and diverse clinical data could be used to build AI tools that are not only technically strong but also clinically relevant across different healthcare systems.
“Its ability to support diagnosis in varied real-world settings, including in Europe, is a step forward in making dermatological expertise more accessible and consistent worldwide,” Professor Kittler said.
PanDerm is currently in the evaluation phase before broader healthcare implementation.
Looking to the future, the researchers aim to develop more comprehensive evaluation frameworks that address a wider range of dermatological conditions and clinical variants.
The team plans to establish standardised protocols for cross-demographic assessments and further investigate the model’s performance in varied real-world clinical settings, with a particular focus on ensuring equitable performance across different patient populations and healthcare environments.
Meanwhile, the authors also believe their research has the potential to impact specialties far beyond dermatology.
“These findings suggest promising directions for developing foundation models in other medical specialties in which the integration of diverse imaging modalities and complex clinical workflows is crucial for patient care,” they concluded.




