A new global consensus exercise yields agreement on 21 factors associated with alopecia areata severity beyond only scalp hair loss.
Judging alopecia severity purely on scalp hair loss alone could soon be a thing of the past.
Existing measures of alopecia severity, like the Severity of Alopecia Tool, primarily focus on scalp hair loss and pay less attention to hair loss in other areas or the psychosocial impact of the condition.
The narrow focus of these measures makes it challenging to accurately capture the multidimensional burden of alopecia areata, which in turn makes it difficult to identify which patients may benefit from current and emerging therapies in an equitable fashion.
Now, a group of international hair and scalp disorder specialists have agreed on 21 factors associated with alopecia areata beyond just scalp hair loss, which will support the development of the Alopecia Areata Severity and Morbidity Index (ASAMI). The findings of the consensus exercise were published in JAMA Dermatology.
“The ASAMI study provides international expert consensus on factors that modulate AA disease severity and insight into current experts’ thresholds for the initiation of systemic treatment,” the authors concluded.
“Identification of determinants of AA severity is the first step toward development of the ASAMI tool: a proposed international expert defined clinical assessment tool for AA.”
Seventy-four experts from six continents were invited to participate in a three-round eDelphi process to achieve consensus on 107 questions and statements about various factors affecting AA severity.
After the final round of the process the experts achieved consensus (66% agreement or disagreement) on 21 questions across four main categories: disease surface area, disease activity, disease visibility and psychosocial morbidity.
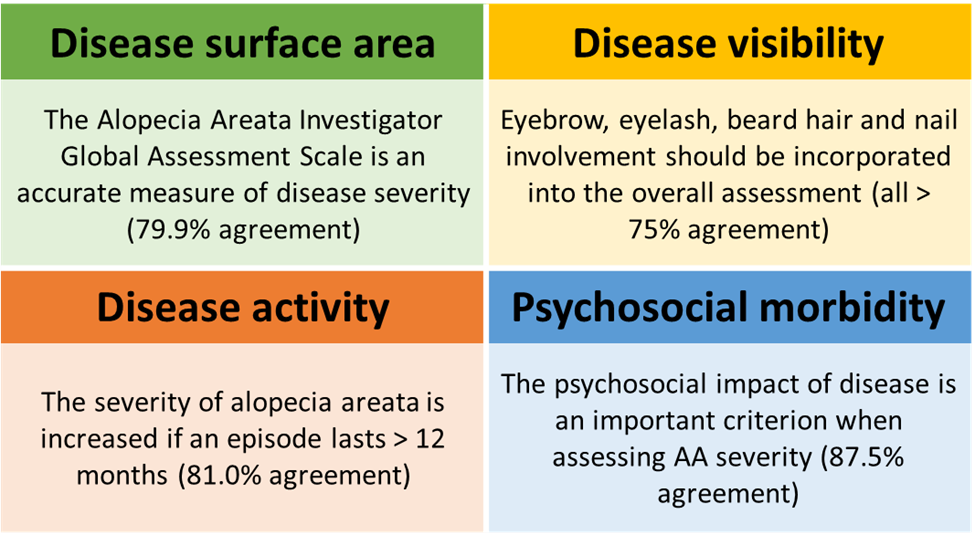
Examples of key consensus outcomes on factors affecting alopecia areata disease severity
There was agreement that patients must experience an episode of AA lasting for at least six months before they become eligible for systemic treatment, and that systemic treatment should not be limited by a longer episode of AA.
The experts agreed the eyebrow, eyelash and nail specific ClinRO measures could be used to assess the severity of disease in these areas. No specific tool was recommended for assessing the severity of beard hair involvement.
In contrast, the authors felt the Dermatology Quality of Life Index was not able to adequately assess quality of life in patients with AA, despite being frequently used to do so. However, they agreed the DQLI score can contribute to the overall severity of AA given a more acceptable tool does not exist.
“The psychosocial impact of AA was underscored by near-unanimous agreement that a history of anxiety, depression or suicidal ideation due to or exacerbated by AA sufficed for systemic treatment initiation,” the authors wrote.
The authors hope the findings of the current study will act as a catalyst for ASAMI development, which will ultimately serve to assess alopecia areata severity, enhance the understanding of disease burden and assist in identifying suitable individuals for new and existing therapies.
“Future research must assign weight to each of the domains that have been identified as contributing to AA severity. Patient and public involvement will be essential in this pursuit, capturing the voices of those who live with AA,” they wrote.


